Lumps and bumps in the palm of the hand are very common. Patients should seek evaluation by a trained physician to make the diagnosis. Below are the most common causes of lumps in the palm.
Ganglion Cyst
The most common cause of a hand lump in the palm of the hand is a ganglion cyst. These are fluid filled sacs which come from the joint or tendon fluid in the hand. Ganglion cysts are not cancer. They often fluctuate in size and can go away on their own. If the cyst is painful, it can be drained with a needle by a doctor or removed by a hand surgeon. Drainage of the cyst with a needle is a simple treatment in the office, but the cyst comes back about 50% of the time. After surgery, the chance of recurrence is 5-10%. If the cyst is not painful or bothersome, it does not require treatment.
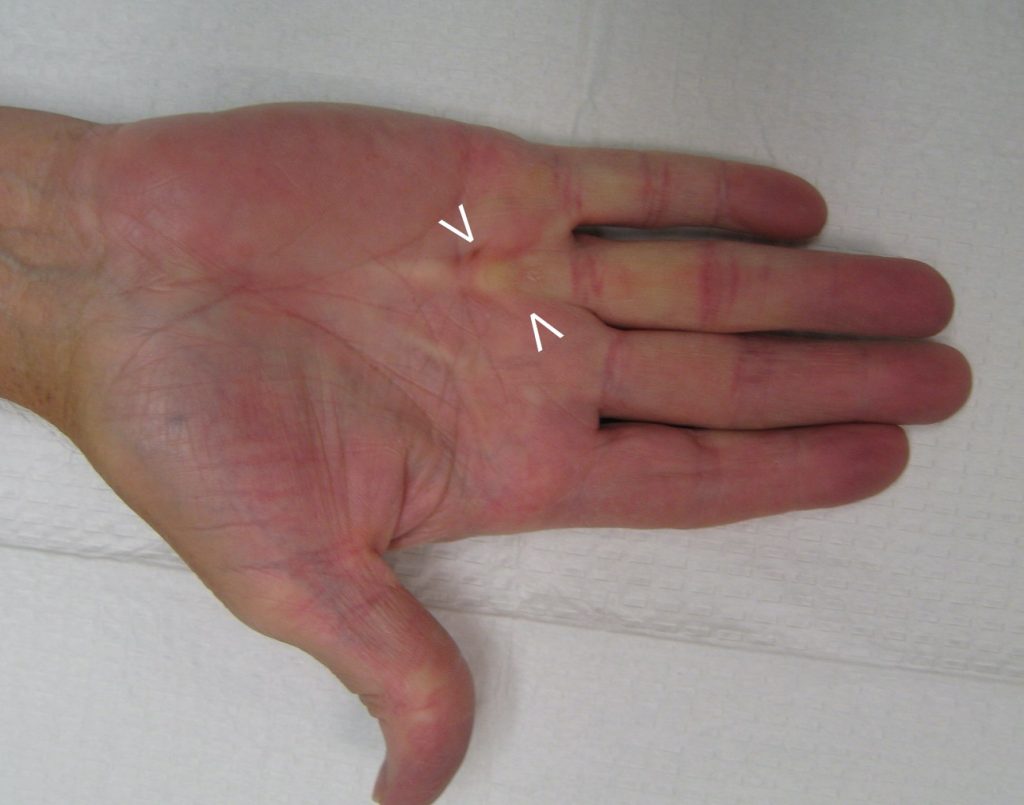
Dupuytren’s Nodule
Another very common cause for a lump in the palm is due to Dupuytren’s disease. These lumps are called Dupuytren’s nodules. Dupuytren’s nodules are made up of abnormal scar tissue. Dupuytren’s is more common in males of Caucasian ethnicity. Sometimes it is called Viking’s disease because it is prevalent in Scandinavian, Scotch-Irish, and Northern European populations where the Viking’s lived. In many cases the condition occurs in both hands and it runs in families. Most of the time the nodule is not painful, but in some patients it is tender or sore to the touch. Tender nodules can be injected with steroid to reduce the soreness and size of the nodule.
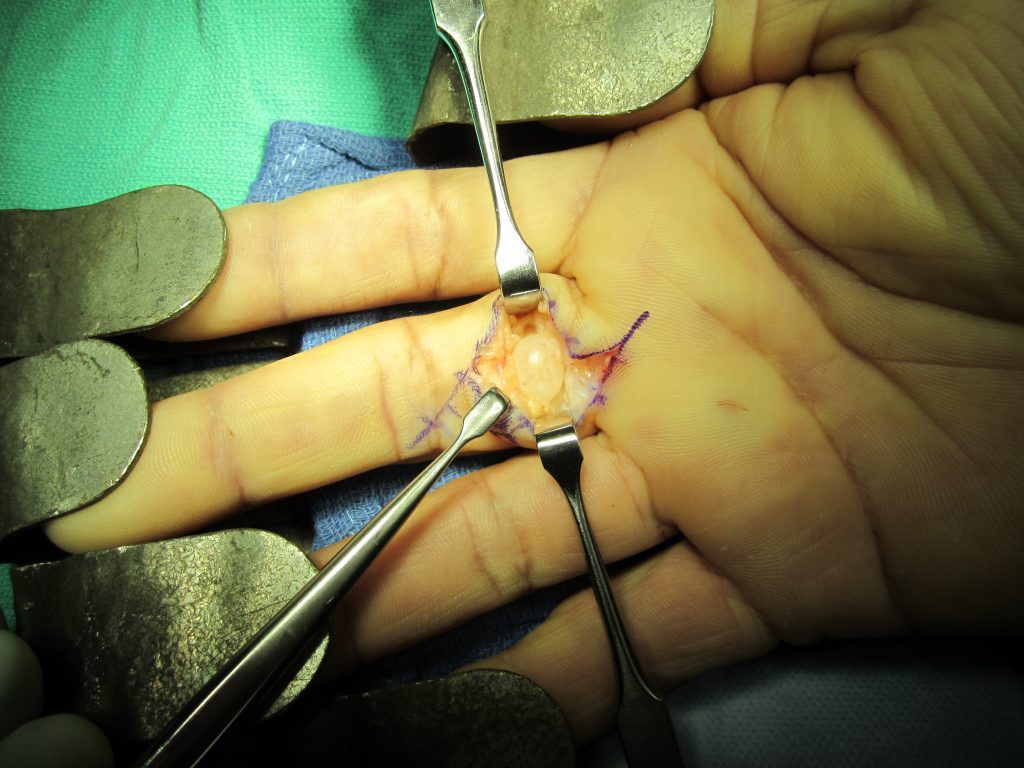
Giant Cell Tumor of Tendon Sheath
Giant Cell Tumors are common tumors in the hand. These are typically firm and slow growing. They can be painful if they press on a nerve or grow to a large size. They are not cancer. Usually these are treated by a surgeon with excision in the operating room. These tumors may come back after surgery. The cause of these tumors is not known but they are usually near a joint or tendon in the hand.
Epidermal Inclusion Cyst
Epidermal Inclusion Cysts are common following trauma or lacerations to the skin of the hand. These are usually slow growing and occasionally tender. These cysts are made of up keratin material shed from skin cells within the lesion. This is a thick, white-yellow, cheese-like substance. Surgery is usually recommended for epidermal inclusion cysts. Recurrence of the cyst after surgery is very low.
There are several other causes for lumps in the palm including: lipomas, nerve tumors, neuromas, blood vessel tumors, and cancers. Please seek evaluation with a trained physician to make the diagnosis. Hand surgeons are experts in the diagnosis and treatment of hand lumps, bumps, cysts, and tumors.
Raleigh Hand to Shoulder Center hand doctors are experts in the diagnosis and treatment of hand disorders including lumps in the palm of the hand. They are top doctors in the field of hand surgery.